Specialties
Degenerative Disc Disease
Our Goal for You:
- Identify the cause of your pain.
- Minimize your down time with non-surgical or minimally invasive procedures if possible.
- Get back to living the life you want.
Overview
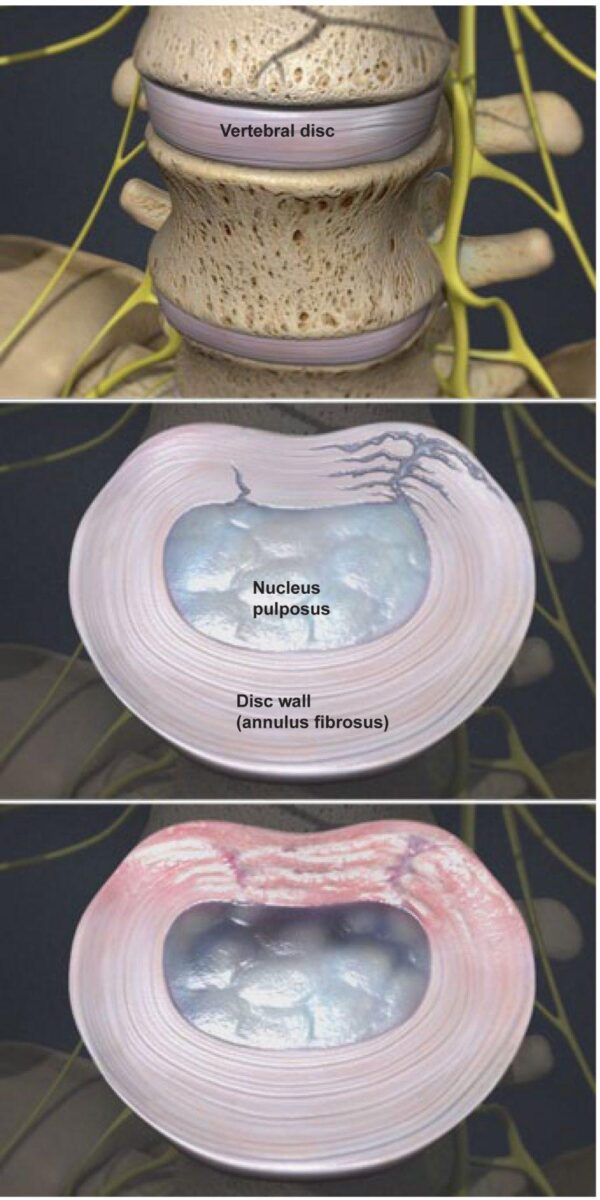
This condition is a weakening of one or more vertebral discs, which normally act as a cushion between the vertebrae. This condition can develop as a natural part of the aging process, but it may also result from injury to the back.
Disc Wall Tears
Degenerative disc disease typically begins when small tears appear in the disc wall, called the annulus. These tears can cause pain.
Disc Wall Heals
When the tears heal, creating scar tissue that is not as strong as the original disc wall. If the back is repeatedly injured, the process of tearing and scarring may continue, weakening the disc wall.
Disc Center Weakens
Over time, the nucleus (or center) of the disc becomes damaged and loses some of its water content. This center is called the pulposus, and its water content is needed to keep the disc functioning as a shock absorber for the spine.
Nucleus Collapses
Unable to act as a cushion, the nucleus collapses. The vertebrae above and below this damaged disc slide closer together. This improper alignment causes the facet joints – the areas where the vertebral bones touch – to twist into an unnatural position.
Bone Spurs Form
In time, this awkward positioning of the vertebrae may create bone spurs. If these spurs grow into the spinal canal, they may pinch the spinal cord and nerves (a condition called spinal stenosis). The site of the injury may be painful.
Symptoms
Some people experience pain, numbness or tingling in the legs. Strong pain tends to come and go. Bending, twisting and sitting may make the pain worse. Lying down relieves pressure on the spine.
Why Choose Advanced Spine Centers
Board Certified & Fellowship Trained.
Voted 2019’s Best Spine Surgeon.
Internationally Recognized Trainer to Spine Surgeons.
Pioneer in Non-Surgical & Micro-Surgical Procedures.

Request an Appointment
Common Patient Questions
ExcellentBased on 147 reviews
 Robert AliceaThe doctor and his staff were very welcoming and kind ..explained my issues in detail . Will highly recommend
Robert AliceaThe doctor and his staff were very welcoming and kind ..explained my issues in detail . Will highly recommend German CisnerosEvery visit to Dr. Courtney's office is educational and most beneficial. Dr. Courtney and ALL of his staff are the best!
German CisnerosEvery visit to Dr. Courtney's office is educational and most beneficial. Dr. Courtney and ALL of his staff are the best! Jamey DerryberryMy wife and I both go to Dr Courtney for back issues. Great care. Great staff. Great surgical facility and smooth process. LOVE THEM!!!
Jamey DerryberryMy wife and I both go to Dr Courtney for back issues. Great care. Great staff. Great surgical facility and smooth process. LOVE THEM!!! Mark CotterDr Courtney and his staff truly care about my well being. They are the only ones I have found that have been able to help me with my workman's comp claim
Mark CotterDr Courtney and his staff truly care about my well being. They are the only ones I have found that have been able to help me with my workman's comp claim J “JAFO”Does your back hurt? Has your back been hurting, yet no other surgeon can or won't help you; or worse tells you nothing is wrong? You're in the wrong place! I had 4 back operations with no improvement. I had an additional 6 other consultations with "there's nothing wrong with you". The truth was I was probably 2-3 months away from permanent leg and lower back paralysis. He fixed me. I can stand, I can walk. I threw away my crutches of 13 years. If you need back correction - GO SEE THIS DOCTOR! He will fix you, and fix you correctly, if it is humanly possible. Enough said! Go see him. He tells the truth and tells it like it is. 🙂
J “JAFO”Does your back hurt? Has your back been hurting, yet no other surgeon can or won't help you; or worse tells you nothing is wrong? You're in the wrong place! I had 4 back operations with no improvement. I had an additional 6 other consultations with "there's nothing wrong with you". The truth was I was probably 2-3 months away from permanent leg and lower back paralysis. He fixed me. I can stand, I can walk. I threw away my crutches of 13 years. If you need back correction - GO SEE THIS DOCTOR! He will fix you, and fix you correctly, if it is humanly possible. Enough said! Go see him. He tells the truth and tells it like it is. 🙂 Terri StewmanDr courtney and his staff are great! Dr courtney always takes his time with you and I feel he truly cares about his patients.
Terri StewmanDr courtney and his staff are great! Dr courtney always takes his time with you and I feel he truly cares about his patients. Ross WigingtonGreat Dr and helped me multiple times over the years Would recommend to anyone that needs help
Ross WigingtonGreat Dr and helped me multiple times over the years Would recommend to anyone that needs help Bridgette e MentesanaDr. Courtney is knowledgeable and takes the time to really explain what’s going on and explain why you’re in pain and the several options to correct the issue. I never felt rushed and he was on time to our appointment which is such a rare thing. The rest of the office staff was absolutely top notch. They were really down to earth and so nice, you could tell they liked their jobs and were treated well. It was a very welcoming atmosphere. I felt very comfortable and I knew I was in capable hands just by the way he treated his staff and listened to his patients. Highly recommend.
Bridgette e MentesanaDr. Courtney is knowledgeable and takes the time to really explain what’s going on and explain why you’re in pain and the several options to correct the issue. I never felt rushed and he was on time to our appointment which is such a rare thing. The rest of the office staff was absolutely top notch. They were really down to earth and so nice, you could tell they liked their jobs and were treated well. It was a very welcoming atmosphere. I felt very comfortable and I knew I was in capable hands just by the way he treated his staff and listened to his patients. Highly recommend. Marie BentonDr Courtney did my neck surgery and my 360 back surgery. I would not go to another surgeon, he cares about his patients and it shows! His staff is great as well! I trust his opinion and skills 100%
Marie BentonDr Courtney did my neck surgery and my 360 back surgery. I would not go to another surgeon, he cares about his patients and it shows! His staff is great as well! I trust his opinion and skills 100%